Iboga root bark or Tabernanthe iboga root bark derived from the Tabernanthe iboga shrub native to Central and West Africa, has been used for centuries in traditional medicine and spiritual practices. The psychoactive properties of the iboga plant have recently garnered attention for their potential in treating addiction, particularly opioid dependence, as ibogaine alleviates drug craving. So, in this article, we will look at Iboga Root Bark For Addiction and its effects.
This article aims to explore the pharmacological effects of iboga alkaloids found in the root bark and how they can be utilized to treat substance misuse disorders, with a focus on heroin addiction. The discussion will delve into the role of brain research in understanding the mechanisms of iboga, its classification as a controlled substance, and its promising potential as an alternative therapy.

Table of Contents
What is iboga root bark?
Iboga, scientifically known as Tabernanthe iboga, is a perennial rainforest shrub native to Central Africa. The root bark of the iboga plant has gained attention for its potential in treating various forms of addiction, particularly heroin addiction.
The iboga root bark is the dried bark of the roots of the Tabernanthe iboga plant. To simplify this definition, it is the shavings of the barks of the roots of the Tabernanthe iboga plant. This plant, native to Central Africa, has been used in traditional ceremonies and healing practices for centuries.
The bark is rich in ibogaine, a powerful psychoactive alkaloid that is the primary active ingredient. Ibogaine is known for its unique effects on the brain, including altering consciousness, reducing cravings, and promoting introspection.
Iboga Root Bark Addiction Treatment: A Comprehensive Guide
The iboga root bark is the dried root bark of the Tabernanthe iboga plant, which grows in the rainforests of West Africa and Central Africa. It is used during spiritual ceremonies.
Iboga root barks contain ibogaine, a psychoactive alkaloid that has been shown to have anti-addictive properties. In traditional African healing practices, iboga root bark has been used to induce vision and as a treatment for a variety of physical and psychological conditions.
Ibogaine alleviated drug cravings in individuals undergoing treatment, making it a significant component of addiction therapy.
Ibogaine offers a promising avenue for treating substance misuse, including heroin addiction, by leveraging its unique pharmacological effects. However, the safety precautions, contraindications, and potential drug interactions underscore the need for a cautious and well-regulated approach.
Continuous brain research into iboga alkaloids will further elucidate their mechanisms and improve the safety and efficacy of ibogaine therapy. Ensuring that treatment is administered within a comprehensive care framework, with attention to medical, psychological, and legal aspects, will optimize outcomes for individuals struggling with addiction.
Ibogaine’s Role in Modern Medicine
Ibogaine, the primary active ingredient in iboga root bark, has transitioned from traditional use to contemporary medical practice. Recognized for its potential to treat addiction, ibogaine has become a subject of interest in modern medicine. Researchers and clinicians are exploring its use in treating opioid dependence, alcohol use disorder, and other substance use disorders.
The transition to modern medicine began in the 1960s when anecdotal reports of ibogaine’s anti-addictive properties caught the attention of Western scientists. Subsequent research has focused on its unique ability to disrupt addiction cycles, offering hope where traditional methods sometimes fall short.
Ibogaine’s role in modern medicine represents a blend of traditional wisdom and cutting-edge scientific inquiry. Studies have shown that ibogaine alleviated drug craving, highlighting its impact on addiction treatment.
Drug Addiction
Drug addiction remains a complex and challenging issue that affects individuals across all demographics and socioeconomic backgrounds. The misuse of various substances, such as opioids, stimulants, and sedatives, can lead to profound physical and psychological dependence, often culminating in addiction.
The American Journal of Medicine highlights the detrimental impact of substance misuse on both individual health and broader societal structures. Medical professionals and researchers continue to explore innovative strategies to address the multifaceted nature of drug addiction, emphasizing the importance of early intervention, comprehensive treatment programs, and ongoing support systems.
Ibogaine alleviated drug craving has shown significant promise in addiction treatment, particularly in reducing withdrawal symptoms and aiding in opioid detoxification.
The practical dangers associated with drug addiction are manifold, ranging from acute health risks to long-term consequences. Overdose, a prevalent risk among individuals struggling with substance use disorders, can result in respiratory depression, cardiac arrest, and even death. Infectious diseases, such as HIV and hepatitis, are also common among individuals who engage in unsafe drug-related behaviors.
Furthermore, the cognitive impairments associated with chronic substance misuse can impact decision-making abilities, impulse control, and overall mental functioning. Efforts to combat drug addiction require a holistic approach that addresses not only the physiological aspects of addiction but also the psychological, social, and environmental factors that contribute to its persistence.
Ibogaine HCl
Ibogaine hydrochloride (HCl) has garnered attention for its potential therapeutic effects in the treatment of substance use disorders, particularly opioid addiction. While animal studies and case reports have shown promising results regarding the efficacy of ibogaine in reducing cravings and withdrawal symptoms, the use of this compound remains controversial due to its classification as a controlled substance.
Ibogaine alleviated drug cravings by significantly reducing both cravings and withdrawal symptoms, making it a promising candidate for addiction treatment.

Regulatory authorities closely monitor the distribution and administration of ibogaine HCl to mitigate the risks of adverse reactions and potential misuse. Individuals considering ibogaine therapy should be aware of the associated safety concerns and seek guidance from healthcare professionals with expertise in this specialized area of treatment.
The availability of iboga products for purchase raises concerns about the quality, purity, and legality of these substances. Buying iboga from unverified sources or without proper oversight can pose significant health risks and legal implications.
As research on ibogaine and its pharmacological effects continues to evolve, it is essential for individuals interested in exploring this treatment option to engage in informed discussions with healthcare providers and addiction specialists. The therapeutic potential of ibogaine HCl underscores the need for rigorous clinical trials and comprehensive monitoring to ensure its safe and effective integration into mainstream addiction treatment modalities.
You also want to read about Iboga Root Bark vs Iboga TA vs Ibogaine HCL: Which to Choose? This is if you want to know which of the iboga forms gives the best result as far as addiction treatment is concerned.
How Does Iboga Root Bark Work to Treat Addiction?
Ibogaine treatment
Ibogaine, the primary active ingredient in iboga root bark, works by interacting with the brain’s reward system, specifically the dopamine receptors. Addiction is often characterized by an imbalance in the brain’s reward system, causing individuals to crave drugs or alcohol.
Ibogaine has been shown to help reset the brain’s reward system, reducing cravings and withdrawal symptoms. It can be taken in high as well as low doses for effective results. It is always administered by trained healthcare professionals to avoid life-threatening complications. Ibogaine alleviates drug cravings by reducing both cravings and withdrawal symptoms, making it a promising option for addiction treatment.
Ibogaine HCL interaction with dopamine receptors is pivotal. It blocks the receptors temporarily, which helps to diminish cravings and interrupts the compulsive cycle of drug-seeking behavior. Additionally, ibogaine’s effects on serotonin and NMDA receptors contribute to its ability to modulate mood and cognitive processes, offering a comprehensive approach to treating addiction.
Psychoactive Properties and Hallucinogenic Effects
Ibogaine’s hallucinogenic effects are integral to its therapeutic potential. During therapy, patients undergo intense, vivid experiences that can last for hours. These experiences help individuals confront underlying psychological issues contributing to their addiction, leading to significant behavioral and emotional changes.
The hallucinogenic journey often includes profound introspection and emotional release. Patients report revisiting past traumas and gaining new perspectives on their lives and behavior.
This psychospiritual experience can lead to catharsis and a strong motivation to change, making it a powerful component of ibogaine therapy. Additionally, studies have shown that ibogaine alleviated drug craving, which is crucial in addiction treatment, particularly for opioid detoxification and substance dependence.
Ibogaine’s Mechanisms of Action
Ibogaine’s mechanisms of action are complex and not yet fully understood. Ibogaine alleviated drug cravings in persons who suffered from addictions. Ibogaine is known to interact with several neurotransmitter systems, including serotonin, dopamine, and NMDA receptors.
This interaction helps to reset the brain’s reward pathways, which are often disrupted by chronic substance abuse. By normalizing these pathways, ibogaine helps reduce cravings and withdrawal symptoms, helps solve drug and alcohol abuse and opioid addiction, and supports long-term recovery from addiction. Ibogaine alleviated drug craving, making it a promising option in addiction treatment.
Ibogaine and the Central Nervous System
Ibogaine’s impact on the central nervous system is a crucial aspect of its effectiveness in treating addiction.
It modulates neural circuits involved in reward, motivation, and stress response, which are often dysregulated in individuals with substance use disorders. By restoring balance to these circuits, ibogaine helps to mitigate the compulsive behaviors associated with addiction and drug dependence and also supports overall mental health.
Ibogaine alleviates drug cravings by reducing cravings and withdrawal symptoms, making it a promising option for addiction treatment.
Neurological and Pharmacological Mechanisms Behind Ibogaine’s Purported Effects
Ibogaine, a naturally occurring psychoactive substance derived from the root bark of the iboga plant (Tabernanthe iboga), has gained attention for its potential in treating addiction. Its effectiveness is rooted in its complex interaction with the brain’s neurotransmitter systems and various receptor sites.
Studies have shown that ibogaine alleviates drug cravings, making it a promising option for addiction treatment.
Neurotransmitter System Interaction
Ibogaine’s primary mechanism involves modulation of the brain’s key neurotransmitter systems. It significantly influences the serotonin (5-HT) and dopamine pathways, which play crucial roles in mood regulation and the brain’s reward circuitry. Ibogaine alleviates drug cravings by reducing cravings and withdrawal symptoms, making it a promising option for addiction treatment.
By acting on these pathways, ibogaine can alter mood states and reduce the intense cravings that characterize addiction.
Serotonin System: Ibogaine affects serotonin transporters and receptors, increasing serotonin levels in the brain. This modulation can enhance mood and provide a sense of well-being, which is beneficial in alleviating the depressive states often associated with withdrawal.
Dopamine System: By interacting with dopamine receptors, ibogaine helps normalize the dopamine function disrupted by prolonged substance use. This action can reduce the compulsive behaviors driven by addiction, as dopamine is a key player in the brain’s reward system.
Receptor Interaction
Ibogaine’s interaction with various receptors further elucidates its potential in addiction treatment:
NMDA Receptors: Ibogaine acts as a non-competitive antagonist at N-methyl-D-aspartate (NMDA) receptors. These receptors are involved in synaptic plasticity and memory functions. By inhibiting NMDA receptors, ibogaine can diminish neurotoxicity and neural hyperactivity associated with chronic drug use, helping to alleviate withdrawal symptoms.
Kappa-Opioid Receptors: Ibogaine’s agonist activity at kappa-opioid receptors contributes to its anti-addictive properties. Activation of these receptors can induce a state that reduces cravings and provides relief from the withdrawal symptoms experienced during detoxification.
Additionally, studies have shown that ibogaine alleviated drug craving, highlighting its significant impact on addiction treatment.
Neuroplasticity and Brain Repair –Brain Research and Iboga
Brain research plays a crucial role in elucidating how iboga interacts with the brain to treat substance misuse. Studies have shown that ibogaine targets various neurotransmitter systems, including serotonin, dopamine, and glutamate, which are implicated in addiction pathways.
By modulating these systems, iboga alkaloids may help individuals overcome cravings and withdrawal symptoms associated with heroin addiction. Ibogaine alleviated drug cravings by reducing cravings and withdrawal symptoms, making it a promising option for addiction treatment.
Ibogaine’s ability to promote neuroplasticity is a critical aspect of its therapeutic potential. It stimulates the release of brain-derived neurotrophic factor (BDNF), a protein that supports the survival and growth of neurons.
This neurotrophic effect can help repair neural damage caused by substance abuse, facilitating the brain’s recovery and improving cognitive functions. The enhancement of neuroplasticity aids in reestablishing healthier neural connections and behaviors, which is essential for long-term recovery.
Psychological and Behavioral Effects
In addition to its biochemical actions, ibogaine induces an intense and often introspective psychological experience. Users report vivid visions and deep self-reflection, which can provide insights into the underlying issues driving their addiction.
This psycho-spiritual aspect of ibogaine therapy is believed to contribute to its effectiveness by fostering a transformative experience that motivates individuals to change their behavior and lifestyle. Furthermore, studies have shown that ibogaine alleviated drug craving, significantly impacting addiction treatment by reducing withdrawal symptoms and aiding in opioid detoxification and substance dependence.
Benefits of Iboga Root Bark in Addiction Treatment
Promotes Long-Term Recovery
Ibogaine has been shown to provide long-term relief from addiction. Unlike traditional treatments requiring ongoing therapy and medication, a single iboga treatment can reduce cravings and withdrawal symptoms for months or even years.
Ibogaine alleviates drug cravings by targeting the brain’s neuropharmacology, significantly reducing cravings and withdrawal symptoms, which promotes long-term recovery.
Studies indicate that ibogaine’s effects can last for extended periods, with many patients experiencing reduced cravings and improved mental clarity for months post-treatment. This long-lasting effect reduces the need for continuous medication, making ibogaine a cost-effective and sustainable treatment option.
Heroin Addiction and Iboga Treatment
Heroin addiction is a complex disorder characterized by compulsive drug-seeking behavior despite harmful consequences. Traditional treatment methods often involve medication-assisted therapies and behavioral interventions.
However, iboga therapy offers a promising alternative for individuals struggling with heroin addiction. The ability of iboga alkaloids to address both physical withdrawal symptoms and psychological cravings makes it a unique candidate for addiction treatment. Additionally, studies have shown that ibogaine alleviated drug craving, highlighting its significant impact on reducing addiction and aiding in long-term recovery.
Addresses Underlying Psychological Issues
Ibogaine helps individuals address underlying psychological issues like trauma, depression, and anxiety, providing a holistic approach to addiction treatment. Ibogaine alleviates drug cravings by reducing cravings and withdrawal symptoms, making it a valuable tool in addiction therapy.
The introspective journey facilitated by ibogaine allows patients to confront deep-seated emotional issues that often fuel addictive behaviors. By resolving these psychological issues, ibogaine therapy supports a more comprehensive and enduring recovery.
Addressing Drug and Alcohol Abuse
Ibogaine therapy addresses both the physical and psychological components of addiction. Patients often report transformative experiences, leading to renewed purpose and commitment to sobriety. Ibogaine alleviated drug craving, significantly impacting addiction treatment by reducing withdrawal symptoms and aiding in opioid detoxification.
The holistic nature of ibogaine therapy ensures that it tackles addiction from multiple angles. Patients not only experience physical relief from withdrawal but also gain emotional and psychological insights that empower them to maintain sobriety.
Iboga Root Bark for Opioid Addiction and Withdrawal
Iboga root bark, particularly through its active compound ibogaine, has gained significant attention in brain research for its potential to treat substance misuse, and drug abuse, including heroin addiction. The pharmacological effects of ibogaine on the brain are profound, involving multiple neurotransmitter systems.
By modulating serotonin and dopamine pathways, ibogaine helps to reset the brain’s reward system, reducing cravings and alleviating withdrawal symptoms associated with opioid addiction.
This reset is crucial in managing heroin addiction, as it addresses the neurochemical imbalances caused by prolonged substance misuse. Ibogaine alleviated drug craving and withdrawal symptoms, making it a promising option for reducing cravings and aiding in addiction recovery.
Ibogaine’s action as a non-competitive antagonist at NMDA receptors further aids in reducing neurotoxic damage and hyperactivity, which are common during withdrawal. This pharmacological effect helps to mitigate the severe physical and psychological distress experienced during opioid detoxification.
Additionally, ibogaine interacts with kappa-opioid receptors, reducing cravings and improving mood, which are critical factors in preventing relapse. Comprehensive brain research continues to explore these pharmacological effects, highlighting ibogaine’s potential to disrupt the cycle of addiction and provide a holistic treatment approach.
However, it’s important to note that ibogaine is a controlled substance in many regions due to its potent effects and potential risks. Therefore, its use to treat substance misuse must be under close medical supervision by medical professionals to ensure safety and efficacy. This is to avoid complications and toxic effects of the iboga shrub due to high doses.
Iboga’s Potential for PTSD and Other Mental Health Conditions
Beyond its application in treating substance misuse or treating drug dependence, iboga root bark has shown promise in addressing mental health conditions such as PTSD. Brain research into iboga alkaloids has revealed their significant pharmacological effects on the brain’s neurochemistry.
For PTSD, ibogaine’s modulation of serotonin and dopamine pathways helps to rebalance mood and alleviate symptoms of anxiety and depression, which are common in trauma survivors. Ibogaine alleviates drug craving, making it a valuable tool in addiction treatment by reducing withdrawal symptoms and supporting long-term recovery.
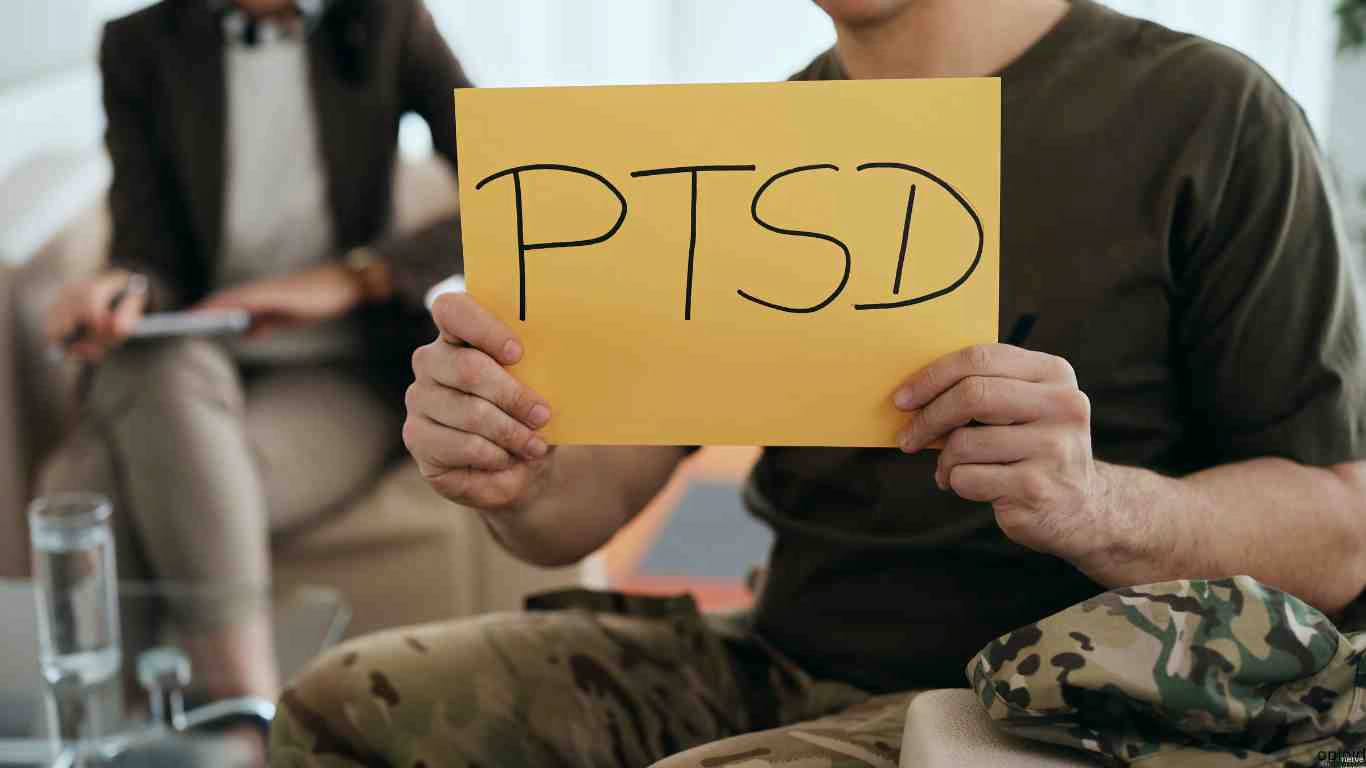
Ibogaine’s ability to promote neuroplasticity through the release of brain-derived neurotrophic factor (BDNF) supports the brain’s healing process, forming new neural connections that can counteract the effects of trauma. This neuroplasticity is particularly beneficial for treating PTSD, where trauma has led to maladaptive neural patterns.
The pharmacological effects of iboga alkaloids in promoting introspection and emotional processing also enable individuals to confront and integrate traumatic experiences effectively.
Additionally, ibogaine’s potential to treat substance misuse and heroin addiction extends to its ability to address co-occurring mental health conditions. The pharmacological effects on neurotransmitter systems can alleviate symptoms of depression and anxiety, providing a comprehensive treatment approach.
However, ibogaine remains a controlled substance due to its intense psychoactive properties and potential for adverse reactions, necessitating careful medical supervision during treatment.
Continued brain research into the pharmacological effects of iboga alkaloids is essential for optimizing therapeutic protocols and ensuring safe and effective treatment for mental health conditions. This research will enhance our understanding of how ibogaine can be used to treat substance misuse and co-occurring disorders, offering hope for those struggling with complex mental health challenges.
Ibogaine Administration and Dosage
The administration of ibogaine must be carefully managed to ensure safety and efficacy. Treatment providers typically administer ibogaine in a controlled setting, with medical supervision to monitor for potential adverse effects. Dosage is tailored to the individual’s needs, with higher doses used for opioid detoxification and lower doses potentially being effective for maintenance therapy or treating less severe substance use disorders.
Understanding the appropriate ibogaine dose is critical to minimizing the risk of ibogaine intoxication and ensuring successful treatment outcomes. Ibogaine alleviated drug craving, making it a promising option in addiction treatment by reducing withdrawal symptoms and aiding in substance dependence recovery.
Methods of Administration
Iboga root bark can be administered in a variety of ways, including:
Chewing the bark directly
Brewing it into a tea
Taking it in capsule form
Using it as an extract
Ibogaine alleviated drug craving has shown significant potential in addiction treatment, particularly in reducing withdrawal symptoms and aiding in opioid detoxification.
Related: Micro-dosing with Ibogaine
Flood Dose
A flood dose involves taking a high dose of iboga root bark, typically 10-20 grams, in a supervised medical setting. This method is considered the most effective for treating addiction.
The intensity of a flood dose requires careful monitoring. Patients are usually under medical supervision for 24-48 hours to manage any adverse reactions and ensure a safe and effective treatment experience. Studies have shown that ibogaine alleviated drug cravings, significantly reducing cravings and withdrawal symptoms, making it a promising option for addiction treatment.
Microdosing
Microdosing, also known as low-dose ibogaine, involves smaller doses over an extended period, effectively reducing cravings and withdrawal symptoms from substance abuse with less intensity than a flood dose.
Microdosing allows for a gradual approach, which can be particularly beneficial for drug addicts who may not tolerate a flood dose well. This method provides ongoing support for managing cravings and maintaining sobriety. Additionally, studies have shown that ibogaine alleviated drug craving, highlighting its potential benefits in addiction treatment.
Capsules
Iboga root bark can also be taken in capsule form for convenience, though this method may be less effective and should be supervised by a medical professional.

Capsules offer a practical and less intimidating method of administration, making ibogaine more accessible. However, the dosage must be carefully managed to ensure therapeutic efficacy and safety. Ibogaine alleviated drug cravings, reducing both cravings and withdrawal symptoms, which highlights its potential benefits in addiction treatment.
Opioid Dependence and Ibogaine Treatment Outcomes
Ibogaine treatment outcomes have been promising in the realm of opioid dependence. Observational studies and early research indicate that ibogaine can produce long-lasting effects, helping individuals maintain sobriety for extended periods.
Treatment providers note that ibogaine’s effects are multifaceted, impacting both the central nervous system and the psychological aspects of addiction. Patients often report a sense of clarity and a reduction in drug cravings following ibogaine ingestion. Additionally, studies have shown that ibogaine alleviated drug craving, highlighting its significant impact on addiction treatment.
Addressing Opioid Withdrawal Symptoms
Opioid withdrawal symptoms can be severe and debilitating, often leading to relapse. Ibogaine has been shown to alleviate many of these symptoms, providing relief during the acute phase of withdrawal. By modulating the brain’s reward system and neurotransmitter pathways, ibogaine helps to reduce the discomfort associated with opioid detoxification, making it easier for individuals to achieve and maintain sobriety.
Additionally, ibogaine alleviated drug cravings, significantly reducing cravings and withdrawal symptoms, which further supports its potential benefits in addiction treatment.
How does iboga treatment compare to other addiction treatment methods?
Iboga treatment is a type of addiction treatment that involves the use of iboga, a psychoactive plant native to West Africa. Iboga has been used traditionally for medicinal and spiritual purposes for centuries and is believed to have powerful healing properties.
Compared to other addiction treatment methods, such as medication-assisted treatment (MAT), cognitive-behavioral therapy (CBT), and 12-step programs, iboga treatment is relatively new and not as well-studied. Some studies have shown that iboga may be effective in reducing drug cravings and withdrawal symptoms, and in helping people overcome addiction.
However, more research is needed to understand iboga treatment’s potential benefits and risks fully. Notably, ibogaine alleviated drug craving, showing promise in addiction treatment by reducing withdrawal symptoms and aiding in opioid detoxification.
One of the unique features of iboga treatment is that it involves a psychedelic experience, which some people believe can help individuals gain a new perspective on their addiction and provide a spiritual or mystical experience that can be transformative. However, this can also be a potential risk, as the use of psychedelics can be unpredictable and may have adverse effects on some individuals.
Overall, iboga treatment may be a viable option for some individuals struggling with addiction, but it should be approached with caution and under the guidance of a trained healthcare professional. It is important to consider all available treatment options and choose the most appropriate approach for each individual’s unique needs and circumstances.
Ethical Considerations in Ibogaine Therapy
Ethical considerations include informed consent, patient safety, and the need for medically supervised treatment settings. Ensuring patients understand the risks and benefits is crucial for ethical treatment. Ibogaine alleviated drug craving, showing significant potential in addiction treatment by reducing withdrawal symptoms and aiding in opioid detoxification.
Informed consent involves educating patients about the potential risks and benefits of ibogaine therapy, ensuring they make well-informed decisions. Additionally, ethical treatment requires robust medical oversight to manage risks and ensure patient safety.
Ibogaine Therapy Protocols and Best Practices
Protocols for ibogaine therapy include pre-treatment screening, dosage guidelines, monitoring during treatment, and post-treatment care. Best practices ensure safety and efficacy, tailoring treatment to individual needs. A systematic review has to be conducted to avoid practical dangers. Ibogaine alleviated drug craving, showing significant potential in addiction treatment by reducing withdrawal symptoms and aiding in opioid detoxification.
Pre-treatment screening involves comprehensive medical evaluations to identify any contraindications. During treatment, continuous monitoring is essential to manage side effects and complications. Post-treatment care includes support for integration and maintaining sobriety.
Long-Term Outcomes and Follow-Up Care
Long-term outcomes of ibogaine treatment include reduced relapse rates and the need for follow-up care. Integrating ibogaine therapy with ongoing support and rehabilitation is essential for sustained recovery. Additionally, ibogaine alleviates drug cravings, significantly reducing cravings and withdrawal symptoms, which contributes to its potential benefits in addiction treatment.
Follow-up care may involve regular check-ins with healthcare providers, participation in support groups, and ongoing counseling. These measures help reinforce the gains made during ibogaine therapy and support long-term recovery.
Potential Risks and Mitigation Strategies
Safety Precautions, Contraindications, and Drug Interactions of Iboga Root Bark for Addiction Treatment
Iboga root bark, especially its primary active compound ibogaine, has garnered attention in brain research for its potential to treat substance misuse, including heroin addiction. However, the potent pharmacological effects of iboga alkaloids necessitate stringent safety precautions.
Ibogaine, a controlled substance in many regions, requires administration under professional medical supervision to mitigate risks. It should be noted that Ibogaine works and should be administered by healthcare professionals. Additionally, studies have shown that ibogaine alleviated drug cravings, significantly reducing cravings and withdrawal symptoms, making it a promising option in addiction treatment.
Safety Precautions
Due to its intense pharmacological effects on the central nervous system, ibogaine treatment mandates careful monitoring. Medical professionals should conduct comprehensive health evaluations, including cardiovascular assessments, as ibogaine can provoke arrhythmias and other serious cardiac issues.
Additionally, liver function tests are essential since ibogaine is metabolized by the liver, and any pre-existing liver conditions can exacerbate potential toxicity.
Furthermore, studies have shown that ibogaine alleviated drug craving, making it a promising option in addiction treatment by reducing withdrawal symptoms and aiding in opioid detoxification.
Contraindications
Certain populations should avoid ibogaine due to its pharmacological effects and the risk of adverse reactions. Buying iboga should be under prescription. Individuals with a history of cardiovascular disease, such as arrhythmias or heart disease, are at heightened risk. Those with psychiatric disorders, particularly psychosis or schizophrenia, may experience exacerbation of symptoms due to ibogaine’s profound impact on neurotransmitter systems.
Pregnant women and individuals with epilepsy should also avoid ibogaine due to its unpredictable effects on these conditions.
Additionally, studies have shown that ibogaine alleviated drug cravings, significantly reducing cravings and withdrawal symptoms, which highlights its potential benefits in addiction treatment.
Drug Interactions
Ibogaine can interact with various substances, making it critical to manage potential drug interactions carefully. It has significant interactions with medications affecting the central nervous system, such as antidepressants, antipsychotics, and other psychoactive drugs. These interactions can amplify the pharmacological effects of both ibogaine and concurrent medications, leading to dangerous outcomes.
Furthermore, ibogaine’s impact on the liver enzyme CYP2D6 can alter the metabolism of many drugs, necessitating adjustments in dosages or the discontinuation of certain medications during treatment. Patients undergoing treatment for heroin addiction or other forms of substance misuse must fully disclose their medication and supplement regimens to healthcare providers to avoid adverse interactions.
Comprehensive Care Approach
Given the complex pharmacological effects of iboga alkaloids, a comprehensive care approach is essential for safe treatment. This includes pre-treatment screening, continuous monitoring during administration, and post-treatment support to manage any long-term effects or potential relapse.
Integrating psychological support and counseling can enhance the effectiveness of ibogaine therapy, addressing both the physiological and psychological aspects of substance misuse.
Legal and Ethical Considerations
Ibogaine’s status as a controlled substance adds a layer of legal and ethical considerations to its use in addiction treatment. It is crucial to ensure that all treatments comply with local regulations and that patients are fully informed of the potential risks and benefits.
Ethical practices involve obtaining informed consent, maintaining transparency about the treatment process, and ensuring that patients have access to follow-up care and support.
Acute opioid withdrawal
Acute opioid withdrawal is a severe and often debilitating condition characterized by symptoms such as nausea, vomiting, muscle aches, and intense cravings. Clinical trials have explored various treatments for managing these symptoms, with ibogaine ingestion emerging as a potential option. Derived from medicinal plants, ibogaine has been the focus of psychedelic research due to its unique properties that may alleviate withdrawal symptoms.
However, the use of ibogaine is not without risks; concerns about ibogaine toxicity and ibogaine intoxication have been highlighted in several studies. Despite these risks, ongoing clinical trials continue to investigate the therapeutic potential of ibogaine and other psychedelic compounds, aiming to establish safe and effective protocols for their use in treating acute opioid withdrawal.

The Future of Ibogaine Research and Therapy
The future of ibogaine research and therapy looks promising, with emerging trends and new applications. Ongoing scientific investigation is essential to realize ibogaine’s therapeutic potential fully.
Future research directions include large-scale clinical trials to establish standardized protocols, exploring ibogaine’s potential for treating other mental health conditions, and developing synthetic analogs that retain therapeutic benefits with reduced risks.
How many people have died from ibogaine treatment?
The number of deaths attributed to ibogaine is relatively small but significant, given its use in addiction treatment. As of recent reports, there have been approximately 20 to 30 documented cases of fatalities associated with ibogaine treatment over the past few decades.
These deaths are often linked to pre-existing health conditions, inadequate medical supervision, and improper dosing. It is crucial to note that while ibogaine shows promise as a treatment for addiction, its administration must be conducted under strict medical supervision to mitigate risks and ensure patient safety.
Legal Status and Regulatory Challenges
The legal status of ibogaine varies globally, presenting regulatory challenges. In some countries, ibogaine is classified as a controlled substance, limiting its availability for treatment and research. Regulatory bodies, including the Drug Enforcement Administration (DEA) in the United States, have stringent regulations, impacting the accessibility of ibogaine therapy.
In the United States, ibogaine is classified as a Schedule I drug, indicating a high potential for abuse and no accepted medical use. However, countries like Mexico, New Zealand, and Brazil allow ibogaine therapy in clinical settings. The disparity in legal status underscores the need for comprehensive research to inform global regulatory frameworks and ensure safe access.
Conclusion
Iboga root bark offers a promising addiction treatment, providing long-term relief from cravings and withdrawal symptoms. However, it carries risks and should be administered under medical supervision. As research progresses, ibogaine therapy may become a valuable tool in the fight against addiction.
The transformative potential of ibogaine therapy underscores the importance of continued research and thoughtful integration into addiction treatment paradigms. With proper safeguards and ongoing investigation, ibogaine could revolutionize the way we approach addiction treatment.
If you’re exploring this route, you can find Ibogaine for sale from trusted sources like us, but it’s crucial to consult with experienced professionals to ensure safety and efficacy.
Resources
National Institute on Drug Abuse (NIDA): NIDA is a government-funded research organization that provides information and resources on addiction and substance abuse. Their website offers resources specifically tailored to the pandemic, including information on telehealth and online support groups.
Substance Abuse and Mental Health Services Administration (SAMHSA): SAMHSA is a government agency that provides information and resources on addiction and mental health. Their website offers resources specifically tailored to the pandemic, including a national helpline for individuals who are struggling with addiction or mental health issues.
Alcoholics Anonymous (AA): AA is a support group for individuals struggling with alcohol addiction. AA has moved many of its meetings online, providing a safe and accessible way for individuals to connect with others who understand their struggles.
Narcotics Anonymous (NA): NA is a support group for individuals struggling with drug addiction. Like AA, NA has moved many of its meetings online, providing a safe and accessible way for individuals to connect with others who understand their struggles.
Mental health professionals: Mental health professionals such as therapists and counselors can provide individualized support and guidance for individuals struggling with addiction during the pandemic. Many mental health professionals offer teletherapy, a form of therapy conducted over the phone or through video conferencing.


